|
| Lorenzo's Oil DVD Cover |
|
| This movie was based on the story of Lorenzo Odone, whose parents searched for a cure for his ALD. |
Support The Myelin Project And The Fight Against Adrenoleukodystrophy
The Myelin Project was founded by parents Augusto Odone and his late wife Michaela. Their son Lorenzo was diagnosed
with adrenoleukodystophy, and since there seemed to be no hope for their son, they took matters into their own hands and did
their own research. They ended up creating a treatment they called "Lorenzo's Oil" that stopped the progression of their
son's illness. (A movie was even made based on their experience titled, not surprisingly, "Lorenzo's Oil".)
Therefore, they have started this organization to continue research into regenerating myelin since the degeneration of myelin
causes adrenoleukodystrophy and a variety of other diseases. This organization specially supports close relations between
families and scientists and is multinational. It allows people to make a difference themselves and help loved ones.
Adrenoleukodystrophy affects approximately 1 in every 17,900 boy worldwide. You can help make a difference in their
lives today by donating to The Myelin Project. This year, we would like to raise 3.2 billion dollars.
But Wait!! What Is Adrenoleukodystrophy Anyway?
Adrenoleukodystrophy is a fairly rare genetic disorder that is caused by the loss of the myelin sheath that surrounds
neurons in the brain, causing the neurons to lose control over muscles and parts of the central nervous system.
In adrenoleukodystophy's worst cases it leaves people who have it in a vegetative state and finally death.
Adrenoleukodystrophy is also characterized by problems with the adrenal gland. It has a common abreviation of ALD, but
it also is called X-linked adrenoleukodystrophy (abbreviated X-ALD), melanodermic leukodystrophy, Schilder's disease, and
sudanophilic leukodystrophy. It was once believed to affect only 1 in every 20,000-50,000 boys, but it is now believed
that it affects 1 in every 17,900 boys worldwide.
What Are Some Of The Types Of Adrenoleukodystrophy And The Symptoms Of These
Types?
- Childhood Cerebral (Demyelinating) ALD- This is one of the most common
forms of ALD and also the most deadly, so it is the form most associated with the name ALD. It usually develops between
the ages of two and ten. Common initial symptoms are problems with school, behavior, vision, and hearing. Unfortunately,
these are often mistaken for conditions like ADHD. This form, along with most of the other forms, also causes
problems with the adrenal gland. After this, the patient deteriorates rapidly into dementia, poor coordination, seizures,
and other symptoms until after about two years the person affected enters a vegetative state and eventually dies.
- Adolescent Cerebral ALD- This form usually occurs between the ages of eleven
and twenty-one. Although it has similar symptoms to the child form, the progression of the diesease is usually not so
rapid.
- Adult Cerebral ALD- This form of ALD is rare, but affects men in their
twenties to fifties. Unfortunately, its progression is rapid and results in a vegetative state or death within
three to four years. The first symptoms appear like those of schizophrenia with dementia.
- Symptomatic Heterozygotes/Female ALD- This type of ALD usually develops
in women after the age of thirty-five. Since women have two X-chromosomes, one can have the defective ALD gene, and
one can have a normal one. They are considered carriers, but they can also show some ALD symptoms. They can be
mild to severe but usually do not cause problems with their adrenal glands.
- Adrenomyeloneuropathy (AMN)- This is a common form of the disease, but
it is usually not life threatening. Originally, affected people show weakness, but then they have adrenal and mental
problems. It usually first manifests symptoms in someone's twenties, but it takes five to fifteen years before they
require the use of a cane or wheelchair.
- Addison's DIsease/Adrenocortical insufficiency- This is technically not
a form of ALD, but most boys and men with ALD have Addison's disease which is sometimes the only sign they have it.
It causes the adrenal gland to not put out enough hormones, but a steroid pill can solve the problem.
- Neonatal Adrenoleukodystrophy (NALD)- This form occurs shortly after birth,
and death usually occurs as a baby or a young child. Some symptoms are seizures and delayed neurological development.
This form can affect males and females. Docosahexanoic acid may help treat this form.
How Life Threatening Is Adrenoleukodystrophy?
People that have the most severe kinds of ALD usually die within one to ten years after their symptoms appear. Before
then, they have progressive neurological problems before spiralling into a vegetative state. Some types, however,
either have a slower progression or just have less serious symptoms in general. Early diagnosis is key, however,
to effectively treating ALD because there is no current way to fix any of the damage of the disease once it is done.
How Do You Get Adrenoleukodystrophy?
Adrenoleukodystrophy is an X-linked recessive trait, which means it mostly affects men. To explain it further, you
must first remember that a woman has two X chromosomes, and a man has one X and one Y chromosome. On the X chromosome
is a gene called ABCD1 that encodes the ALDP (ALD protein) that helps break down very long chain fatty acids. The abnormal
immune response to the accumulation of these very long chain fatty acids results in demyelination. ALD occurs
when this gene is defective in a recessive fashion. Because men have only one X chromosome, if they receive a defective
form of the gene on their X chromosome they should show the disease because they have no other X chromosome to have a normal
dominant gene to cover up the defective recessive one. Because women have two X chromosomes, they can receive one defective
recessive gene and one normal dominant gene to just be considered a carrier. However, they can still develop some of
the milder symptoms of ALD as symptomatic heterozygotes (also called female ALD). If a woman is a carrier, though, she
can still pass on the defective gene to her children, and a son could inherit it. Technically, there is also the slight
chance of a woman getting two defective ALD genes (one from each parent) and show symptoms of a more severe form of ALD, but
this is highly unlikely due to the quick, high mortality rate for most men that get the severe forms of the disease.
How Can You Detect Adrenoleukodystrophy?
Adrenoleukodystrophy can usually be detected by a simple blood test that can tell if someone has the disease by high levels
of very long chain fatty acids. However, this test does not detect about twenty percent of women carriers. A DNA-based
blood test, though, can definitely determine if a woman is a carrier. This test can also be used to detect ALD in boys who
have not yet started showing symptoms. After a blood test shows ALD, usually an MRI will be done to see how much the
brain has already been affected, and another blood test is done to check for adrenal insufficiency because this is a common
symptom of the disease that can be treated. A Loes score (which measures brain damage on an MRI on a scale of zero to
thirty-four) of fourteen or more means the person has severe ALD. Five tenths or below is considered normal.
A prenatal diagnosis or genetic counseling is available for before a baby is even born. Amniocentesis and chorionic
villlus sampling (CVS) can also be used to detect ALD but only if it is specifically looked for. Some signs you can
look for to also indicate the presence of ALD are: late-onset ADHD or other attention problems, especially when the child
does not respond to the medicines for them, adrenal insuffiency or Addison's disease, vision problems, rapid progression of
these changes, and a family history. Early diagnosis is especially critical in ALD because at this time there is
no way to repair ALD damage to the brain after it has occurred.
Does Adrenoleukodystrophy Have Any Cures Or Treatments?
Currently, there is no way to fix damage caused by ALD once it has been done, but there are ways to help ease symptoms
and try to slow down the progression of the disease or even stop the disease from progressing any further.
- Lorenzo's Oil- This is a treatment developed by Augusto and Michaela Odone
after their son Lorenzo developed ALD to slow the progression of his disease. It is made of extracted fats from olive
oil and rapeseed oil. These fats, along with a low fat diet, reduce the amounts of very long chain fatty
acid known to cause ALD. Unfortunately, it only seems to work in keeping symptoms away from boys who have
not developed them yet. This makes results inconclusive because you cannot know for sure whether the boys were to have
ALD at all or will develop another form later.
- Stem Cell Transplantation- In this treatment, stem cells with a healthy
ALD gene taken from bone marrow or umbilical cord blood are transplanted into a patient with ALD, and it is believed these
cells make their way to the brain to make the missing ALD protein and stop or reverse the brain damage. Unfortunately,
there is only a certain time at which this treatment is effective, sometimes the cells are rejected even though
the body is put at risk for infection by wiping out the immune system, and even after the transplant, there is still
six to eighteen months where the disease progresses.
- Replacement Of Adrenal Hormones- This is used when there are problems with
the adrenal glands. Taking a steroid pill can help.
- Symptomatic and Supportive Treatments- These types of treatments deal with
making the patient more comfortable and providing the person and the family with emotional support.
Is There Any Promising Research For Adrenoleukodystrophy?
- Gene Therapy- This technique is being developed where certain cells are
taken out of the patient, and the correct gene is inserted. Then the cells are placed back into the patient to help
make the ALD protein he was lacking. This would be much less risky than a stem cell transplant because patients
get the cells from themselves, so there is no need to wipe out their immune system because there is no risk of rejection.
- Mucomyst (Acetyleysteine)- This drug is currently being tested because
it seems to stop the rapid neurological progression of the disease in patients that already have an advanced form.
- ALDR Upregulation- This idea being studied is that you could incease the
activity of a gene similar to the ALD gene, but ALD patients have a normal copy of it. The increased activity
of this gene could compensate for the defective ALD gene.
- Mesenchymal Stem Cell Therapy- These stem cells are cultured from adults'
bone marrow, but they have the ability to differentiate into many other types of cells. It is believed they
could greatly help ALD patients when they are put into their blood and brains.
- Myelin Restoration- This is research done particularly by The
Myelin Project to find ways to restore lost myelin to reverse ALD brain damage. Two ways of treatment they are looking
at are transplanting myelin-forming cells and finding drugs to replace it.
- 4-phenylbutyrate and Lovastatin- These drugs are being tested because they
could potentially reduce levels of very long chain fatty acids in the brain.
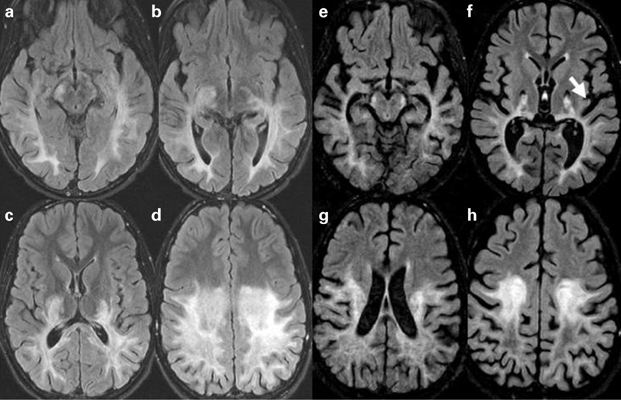
| Bone Marrow Transplant Results |
|
| This picture shows MRIs of a ten year old boy with ALD before (a-d) and after (e-h) transplant. |
|

