|

Children With Diabetes Foundation
The Children With Diabetes Foundation supports clinical efforts which seek to identify those at risk for
developing type I diabetes. We do not provide funding for the prevention of complications studies or studies which rely on
embryonic, fetal, or cloning research.
The Children With Diabetes Foundation would like to raise two million dollars by January of
2009. Please support the CWD Foundation by making a donation. Every donation makes a difference, no matter how small.
What is Type 1 Diabetes?
Before a person can begin
learning about type 1 diabetes, he or she needs to know about glucose, the pancreas, and insulin, and their importance to
the human body. Glucose, a simple sugar, is the main source of energy for the body. The pancreas, which is located under the
stomach, contains hormones that produce insulin. Insulin is what makes it possible for a cell to take in glucose.
Type 1 diabetes affects the
way the body turns glucose into energy. This disorder destroys the hormones located in the pancreas that make insulin. Without
insulin, cells cannot accept glucose. Instead, the glucose builds up in the bloodstream. The lack of glucose in the body’s
cells results in the lack of energy the body can use. The absence of insulin and the building up of glucose also leads to
a high blood sugar, or hyperglycemia.
Type 1 diabetes is a chronic
disease because the body cannot produce its own insulin. Even though there are ways to treat type 1 diabetes, it lasts for
a diagnosed person’s entire life.
There are many symptoms
that show if a person has been affected by type 1 diabetes. A person who has not yet been diagnosed has frequent urination,
sugar in urine, and fruity, sweet, or wine-like odor in breath. Other symptoms are extreme thirst, drowsiness, sudden vision
changes, increased appetite, sudden and drastic weight loss, and heavy breathing.
Type 1 diabetes is known
by a variety of names. The medical term for this disorder is diabetes mellitus. Other names that are often used are juvenile
diabetes, brittle diabetes, unstable diabetes, ketosis-prone diabetes, and insulin-dependent diabetes.

How is Type 1 Diabetes
Passed on Genetically?
Type 1 Diabetes is an
autosomal recessive disorder. This means that in order for a person to be diagnosed with diabetes he or she has to receive
two recessive alleles, one from each parent.
A person’s chance of developing type 1 diabetes is at about two percent
if the mother has the disorder. The chances increase to six percent if the father or a sibling has type 1 diabetes.
Even though genetic inheritance
plays a major part in type 1 diabetes, environmental factors are also involved. Some environmental factors that can affect the development of type 1 diabetes are an excessive
intake of food, too much stress, and viral infections.
Who is Affected by Type 1 Diabetes?
Studies show that about
one in every four hundred children and adolescents are diagnosed with type 1 diabetes. Girls usually develop type 1 diabetes
between the ages of ten and twelve, and boys between the ages of twelve and fourteen. However, more recent studies show that
there is an increase of development of type 1 diabetes in children under the age of four. Caucasians have a higher rate of
developing type 1 diabetes than other ethnic groups.
What is it like to
have Type 1 Diabetes?
Checking Your
Blood Sugar Level
After a person is diagnosed
with type 1 diabetes, the level of glucose in the bloodstream needs to be checked several times a day. The usual times for
checking blood sugar are after waking up, before going to bed, before every meal, and sometimes after meals.
The first step in checking
the blood sugar level is pricking a finger with a needle. Then place a drop of blood on a meter strip. Once there is enough
blood on the strip, the person checking his or her blood sugar level needs to insert the strip into the meter. In a few seconds
the meter will give an accurate blood sugar level.
There are three levels
that a blood sugar reading can be placed. They are euglycemia, hypoglycemia, and hyperglycemia. Euglycemia is a normal blood
sugar level, which ranges from about 75 to 165 mg/dl. When a diabetic’s blood sugar is at this level, he or she feels
happy and energetic. Hypoglycemia, or a low blood sugar, has a meter reading at about 75 mg/dl or under. This level of blood
sugar usually results in a person feeling weak, tired, or shaky. In order to bring the blood sugar back to normal, a person
should consume sugar, check blood sugar, and eat a snack with carbohydrates. When a person’s blood sugar is in the hyperglycemia
level, he or she has a high blood sugar, or a meter reading of about 165mg/dl or above. A diabetic with a high blood sugar
usually feels faint, queasy, and is thirsty, and he or she should take a prescribed dose of insulin and drink water to retrieve
a normal blood sugar reading.
Taking Insulin
People with diabetes
need to inject insulin into a muscle, which then flows into the bloodstream, to keep their body working normally. This process
replaces the insulin that would normally be produced by hormones in the pancreas. The prescribed amount of insulin varies
between each diabetic, but the usual number of daily injections is two.
The
different types of insulin are S or R, N or L, and U. Insulin bottles labeled with an S or an R contain short-acting insulin.
N and L labeled bottles have insulin that is intermediate-acting. U insulin is the longest lasting insulin that can be injected.
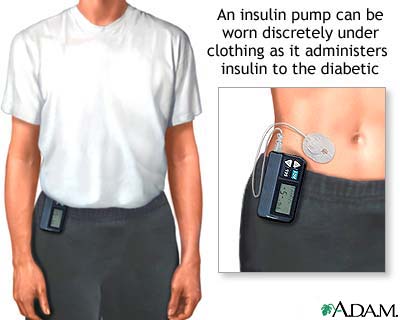
Instead of injecting insulin with shots, diabetics also have
the option of using an insulin pump. An insulin pump is about the size of a beeper, and it connects to a plastic tube and
needle. The needle needs to be replaced every two to three days. The insulin pump holds the prescribed insulin and delivers
a basal rate of insulin, which are small amounts that the pancreas would normally secrete all the time. By pressing a button, the pump can also deliver a bolus of insulin,
which replaces the extra insulin the pancreas would produce after meals.
A Healthy Diet
For diabetics, following
a healthy diet is especially important because food has a big impact on the blood sugar level. When looking at a nutrition
label, a diabetic needs to look at the amount of carbohydrates to help decide the amount of insulin to take.
Even though diabetics
have to watch what they eat more closely, they can still consume all types of foods and drinks like everyone else. The only
extra things diabetics have to do are taking insulin and watching the amount of sugar and carbohydrates in a particular item.
Exercise
Exercise is also beneficial
for diabetics because it helps lower blood sugar levels. Also, the more often a diabetic exercises, the amount of insulin
he or she needs to take is less.
Visiting Your
Doctor and Dietician
Once a person is diagnosed
with diabetes, they must work with an endocrinologist and a dietician to maintain a blood sugar as normal as possible. An
endocrinologist is a doctor that is specialized in diabetes and other hormonal disorders.
A diabetic needs to work
with a dietician to learn how to control blood sugar level through diet, exercise, managing carbohydrate intake, and receiving
proper nutrition.
What Problems are Associated
with Type 1 Diabetes?
Over time type 1
diabetes can lead to blindness, kidney failure, and nerve damage. Type 1 diabetes can also accelerate the hardening and narrowing
of arteries. This can lead to strokes, coronary heart disease, and large blood vessel diseases. Even though a person can die from these problems, there are treatments that can be given to a person with
diabetes if they go to the hospital immediately.
If a diabetic takes checks
his or her blood sugar level regularly and takes insulin when he or she is supposed to, he/she can live the life of an ordinary
human being. Physical limitation can occur only if a diabetic is diagnosed with a complication that resulted from type 1 diabetes.
Diabetes is not an invariably
fatal disorder because there are ways to treat the many complications that diabetes can cause.
Are There any
Cures for Type 1 Diabetes?
Even though there is no
known cure for type 1 diabetes, there are methods that are being researched to achieve the effect of insulin production. The
methods being researched are pancreas transplantation or artificial pancreas development, islet cell transplantation or artificial
development, and genetic manipulation.
Pancreas Transplantation
A diabetic is able to
receive a whole pancreas transplantation. With this procedure a type 1 diabetic is given a donor pancreas. If the transplant
is a success, the patient no longer has type 1 diabetes, therefore does not have to check blood sugar or take insulin. However,
if the body rejects the donor pancreas, the patient continues to be a type 1 diabetic.
When no donor pancreases
are available, a type 1 diabetic can instead receive part of a living relative’s pancreas. The transplant has a higher
chance of success if the patient and the relative have matching HLA types. A patient usually receives a partial pancreas transplant
when he or she is also receiving a kidney transplant.
Pancreas transplants are
recommended for type 1 diabetics who do not have heart or blood vessel disease. After receiving a pancreatic transplant, the
patient has to take certain drugs for the rest of his or her life and needs to avoid people with infections, such as the cold
and the flu.
Islet Cell Transplantation
Islet cell transplantation
is a type of transplant that provides the patient with new islet cells taken from a donated pancreas. This type of transplantation
is recommended for people who have complications with type 1 diabetes or a severe type of 1 diabetes that cannot be treated
with insulin therapy. However, islet cell transplants are not widely available. In the United States it is considered an experimental
transplantation, so a patient might have to wait a while before receiving a donated pancreas. If the transplant is successful,
the amount of insulin taken will be gradually reduced as the new islet cells begin to function.
A type 1 diabetic that
receives an islet cell transplantation is more susceptible to viral and bacterial infections. People who receive this type
of transplant are also at a higher risk of increased blood cholesterol levels,
high blood pressure, decreased kidney function, and an increased risk of tumors and certain types of cancer
Genetic Manipulation
Research for finding a
gene to manipulate and a way to manipulate it has also taken place.
In one study, researchers
used a recombinant adeno-associated virus. This virus was used to transport a single-chain insulin analogue, or SIA, into
the liver of diabetic rodents. The SIA gene has a glucose regulator. Therefore, whenever the glucose level in the blood rises,
the SIA gene is activated, and releases a version of insulin that regulates the blood sugar level. The rodents no longer showed
symptoms of type 1 diabetes after being treated with this genetic therapy. There were also no side effects.
However, problems have
been discovered when inserting the SIA gene into the human body. These problems include failure of the gene to function constantly
over time, failure of the gene to control blood sugar levels, and failure of the gene product to be effectively metabolized
into insulin.
What Tests Can be Performed
to Detect Type 1 Diabetes?
The three main tests used
to detect type 1 diabetes after the patient has shown symptoms are urinalysis, blood work, and continuous testing of blood
sugar level. A urinalysis is used to measure the amount of sugar in the patient’s urine. Blood samples are taken from
the patient to be studied for the amounts of glucose. The blood sugar level of the patient is checked constantly to look for
changes in blood sugar levels.
With the information researchers
have collected so far, doctors can screen a patient for antibodies to insulin or beta cells. The antibodies indicate a high risk for developing type 1 diabetes. These antibodies can be present up to eight
years before symptoms develop. However, because knowing a child's risk does not help prevent type 1 diabetes, the American
Diabetes Association only recommends using these tests in children who have a parent or sibling with diabetes. They also recommend
these tests for those who are entering a scientific study that requires the information.
Is There a Way to Detect
a Carrier of Type 1 Diabetes?
There are no ways to accurately
detect a carrier of type 1 diabetes as of right now. Genetically speaking, the chances of a child being diagnosed with type
1 diabetes are higher if at least one of the parents has the disorder. However, it is possible for a parent with type 1 diabetes
to not have any children that develop the disorder.
|

